Dr. Shilpa Gandhi | Leading Consultant Minimally Invasive Thoracic Surgeon In Nagpur
Meet Our Doctor
Dr. Shilpa Gandhi
MBBS, DNB General Surgery DNB Thoracic Surgery
Dr. Shilpa Gandhi is a trusted and experienced healthcare professional known for her compassionate care and expertise. Committed to delivering personalized treatments and improving patient well-being.

Surgery For Myasthenia Gravis
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder that causes weakness in the voluntary muscles. While there are several treatment options available for managing Myasthenia Gravis, including medications and plasmapheresis, surgery for Myasthenia Gravis can be an important component of the treatment plan, especially in cases that do not respond to medication alone.
In this article, we will explore the role of surgery for Myasthenia Gravis, its benefits, types of surgical procedures, and what patients can expect during their recovery process. If you’re considering surgical treatment for Myasthenia Gravis, this guide provides key insights into your options and the potential outcomes of surgery.
Introduction to Surgery for Myasthenia Gravis
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder that causes weakness in a skeletal muscles. The condition occurs when the body’s immune system attacks the communication between nerves and muscles, leading to muscle weakness and fatigue. While Myasthenia Gravis can often be managed with medications, in some cases, surgery for Myasthenia Gravis offers an important treatment option that can significantly improve a patient’s condition, particularly when medication alone does not a provide sufficient relief.
The most common surgical treatment for Myasthenia Gravis is thymectomy, the removal of a thymus gland. This surgery has shown to offer benefits, particularly in patients with generalized MG, and can help reduce or even eliminate symptoms in certain cases. In this comprehensive guide, we will discuss when surgery for Myasthenia Gravis is recommended, the surgical procedures available, and what patients can expect from the surgery and recovery process.
What is Myasthenia Gravis?
Myasthenia Gravis (MG) is an autoimmune disorder where the body’s immune system mistakenly attacks the neuromuscular junction, where nerves communicate with muscles. This results in muscle weakness, particularly in areas such as the eyes, mouth, throat, and limbs. Patients with MG often experience symptoms like difficulty swallowing, double vision, drooping eyelids, and severe fatigue. These symptoms tend to worsen with physical activity and improve with rest.
When is Surgery for Myasthenia Gravis Recommended?
Surgery for Myasthenia Gravis is not always the first-line treatment, but it may be recommended in specific cases where other treatment options have not been effective. The most common surgical intervention for Myasthenia Gravis is thymectomy, the removal of the thymus gland, which has been shown to improve symptoms in many patients. Surgery may be considered if:
Severe or Inadequately Controlled MG: When symptoms of Myasthenia Gravis are severe or cannot be effectively managed with medications, surgery might be recommended to improve muscle strength and reduce dependency on drugs.
Thymoma: In some cases, patients with Myasthenia Gravis also have a thymoma, a tumor of the thymus gland. Removal of the thymoma, along with the thymus gland itself, can improve MG symptoms and potentially treat the tumor.
Inadequate Response to Medication: If a patient does not respond adequately to anticholinesterase medications, immunosuppressive drugs, or plasmapheresis, surgery might be a necessary option to control the condition.
Younger Patients: Thymectomy has shown the most significant benefit in younger patients (under 60) with generalized Myasthenia Gravis, who may experience long-term improvement in symptoms following surgery.
Types of Surgery for Myasthenia Gravis
There are primarily two types of surgical procedures that can be used to treat Myasthenia Gravis:
1. Thymectomy
Thymectomy is the most common and effective surgery for Myasthenia Gravis. The thymus gland plays a role in the immune system, and its abnormal function is thought to contribute to the development of Myasthenia Gravis. In many cases, removing the thymus gland can lead to an improvement in symptoms, and some patients even experience remission of their condition.
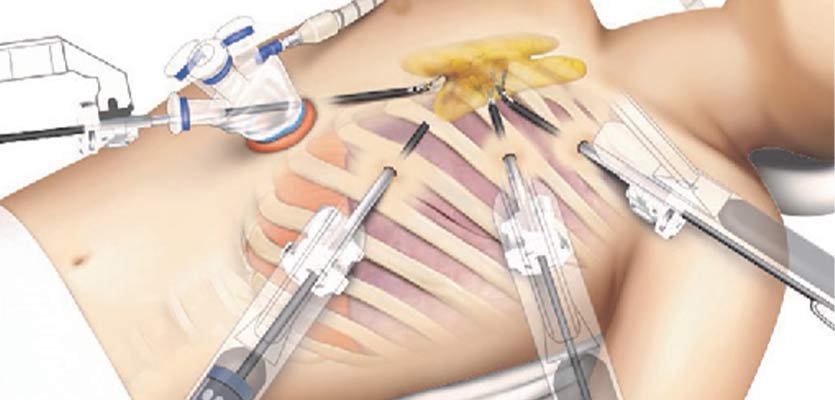
- Procedure: Thymectomy can be performed through a traditional open surgery or minimally invasive techniques like video-assisted thoracoscopic surgery (VATS). In open surgery, an incision is made in the chest to access and remove the thymus, whereas VATS uses smaller incisions and a camera to guide the procedure.
- Benefits: The procedure is associated with improved long-term outcomes for many patients, with a significant reduction in symptoms and, in some cases, complete remission of Myasthenia Gravis. Studies have shown that thymectomy can reduce the need for immunosuppressive drugs and improve overall muscle strength.
- Thymectomy and Thymoma: In patients with thymoma (a tumor in the thymus), thymectomy serves the dual purpose of treating both the tumor and the underlying Myasthenia Gravis. This surgery is essential to prevent cancer spread and improve MG symptoms.
2. Plasmapheresis and IV Immunoglobulin (IVIg) Therapy
While not strictly a surgery for Myasthenia Gravis, plasmapheresis and IVIg therapy are often used in combination with surgery to treat severe symptoms of MG. These treatments are typically used in acute situations where a rapid reduction in disease activity is required.
- Plasmapheresis involves the removal of harmful antibodies from the blood, which can temporarily alleviate symptoms.
- IVIg is an infusion of immunoglobulins (antibodies) from healthy donors that help modulate the immune system and reduce the autoimmune attack on the neuromuscular junction.
These treatments are generally short-term options and are used to stabilize the patient until surgery, such as thymectomy, can take place.
Benefits of Surgery for Myasthenia Gravis
Surgery can offer several significant benefits for patients with Myasthenia Gravis, especially for those with severe or refractory symptoms. Some of the key benefits include:
Long-Term Symptom Relief: For many patients, thymectomy results in long-term improvements in muscle strength and a reduction in symptoms. It can help lessen the need for daily medications and may even lead to complete remission in some cases.
Reduction in Medication Dependence: Surgery can reduce the need for immunosuppressive drugs, which carry significant side effects over time. As the symptoms improve following surgery, patients may be able to reduce or even stop their medications under the guidance of their doctor.
Improved Quality of Life: By improving muscle function and reducing weakness, surgery can significantly improve the overall quality of life for people with Myasthenia Gravis. This includes less fatigue, better speech, improved swallowing, and the ability to perform daily activities without as much difficulty.
Treating Thymoma: If a thymoma is present, thymectomy provides the additional benefit of removing the tumor, preventing potential cancer growth, and reducing the risk of complications related to the tumor.
Reduction of Crisis Episodes: Patients with MG are prone to myasthenic crises, a severe exacerbation of symptoms that can lead to respiratory failure. Surgery can reduce the frequency and severity of these crises, improving patient safety and reducing hospitalizations.
What to Expect During the Recovery Process
Recovery after surgery for Myasthenia Gravis depends on the type of surgery performed, the patient’s overall health, and how well they respond to the procedure. Below is a general outline of the recovery process:
Initial Recovery: After surgery, patients will typically stay in the hospital for several days to monitor for complications such as infection, bleeding, or respiratory issues. Thymectomy patients may require some time in the intensive care unit (ICU) for post-operative monitoring.
Pain Management: Mild to moderate pain is common after surgery, but it can usually be managed with pain medications. Most patients recover from the incision pain within a few weeks.
Rehabilitation and Physical Therapy: After surgery, physical therapy may be recommended to help strengthen weakened muscles and improve mobility. Patients will gradually return to their daily activities as strength improves.
Follow-Up Care: Regular follow-up appointments are necessary to assess recovery, evaluate the patient’s response to surgery, and adjust medications if needed. Blood tests and imaging may be used to monitor for any signs of complications, such as infection or recurrence of thymoma.
Long-Term Outcomes: Many patients experience a gradual improvement in muscle strength over the course of several months. For those who undergo thymectomy, the most noticeable improvements often occur within the first year after surgery, though some patients report improvements even years after the procedure.
Risks and Considerations
Like all surgeries, surgery for Myasthenia Gravis carries some risks. These may include:
- Infection at the surgical site.
- Blood clots, especially in patients with reduced mobility after surgery.
- Breathing difficulties in the case of severe MG symptoms or respiratory muscle weakness.
- Recurrence of Symptoms: In some cases, patients may experience a return of symptoms, especially if surgery is performed at a late stage of disease progression.
Conclusion
Surgery for Myasthenia Gravis, particularly thymectomy, can be an effective treatment option for patients with severe or poorly controlled symptoms. It offers long-term symptom relief, reduces the need for medications, and can significantly improve quality of life. For patients with thymoma, thymectomy also plays a crucial role in treating the tumor and improving the prognosis of both Myasthenia Gravis and cancer.
If you or a loved one has been diagnosed with Myasthenia Gravis, it is important to discuss surgical options with your healthcare provider to determine if surgery is the right approach for your condition. Early intervention with thymectomy or other treatments can make a significant difference in managing the disease and improving long-term health outcomes.



